Lab Communications
Latest updates and alerts
03/07/2025
Critical reagent shortage: Transferrin
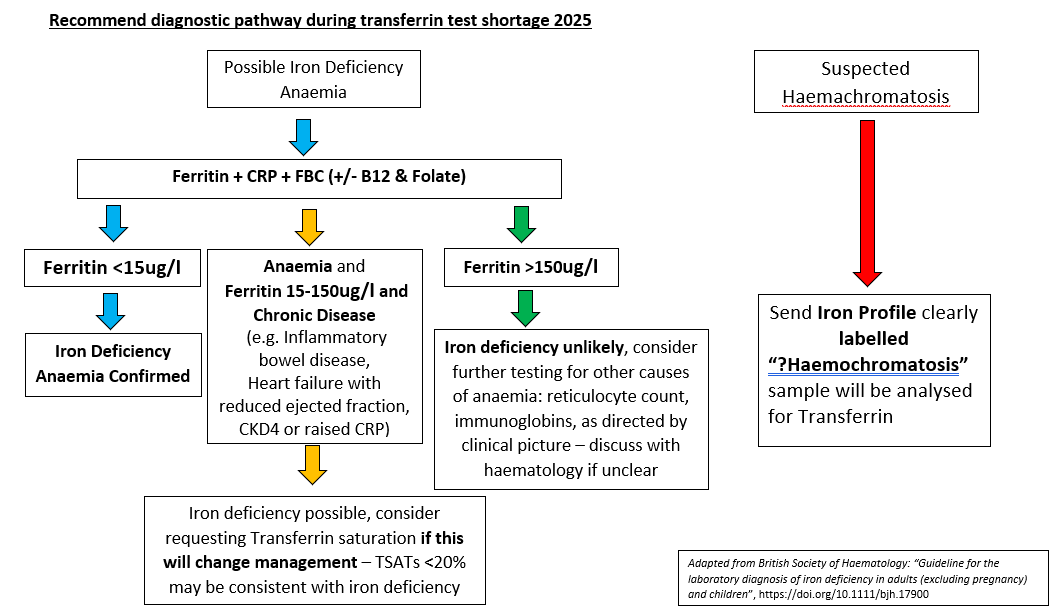
Due to a national reagent shortage, we are compelled to limit the availability of our transferrin assay, which forms part of “iron profile” panel.
Weekly we receive about 1000 requests for “iron profile” analysis alone therefore we ask you to limit the requesting to only necessary testing as per national guidance and provide clear clinical indication for a request.
Transferrin + Transferrin saturation is useful in determining iron loading e.g. hereditary haemochromatosis, or in determining iron status in the setting of inflammation/chronic disease states.
We will analyse transferrin + transferrin saturation on any samples with clinical details indicating clear suspicion of haemochromatosis labelled for the attention of the Duty Biochemist (please highlight).
Any other samples requiring “iron profile” will have only ferritin analysed and stored for 48 hours to allow discussion with Duty Biochemist in cases where transferrin is deemed necessary for clinical management (will change clinical management).
This is a temporary measure to preserve reagent availability and will take place as of today, 3rd July 2025. We anticipate full service to resume by mid- September.
We apologise for the inconvenience this might cause. For urgent clinical need or further information, see below flow chart for interim management. If additional information is required, please contact iain.woodrow@nhs.net, ben.nicholson@nhs.net or cat.dibden@nhs.net.
Monitoring advised as per national guidelines
Ferritin monitoring
- EASL recommends; An initial retesting interval of three months, but this should be tested more frequently as ferritin approaches normal range
- BCSH 2000 recommends: Monthly ferritin during venesection
Iron deficiency diagnosis
- Repeat iron measurement not required unless diagnostic uncertainty
- Check FBC two weeks post-iron therapy
- Once Hb normalised check FBC after two months
Iron status in CKD
- Monitor iron status no earlier than one week after receiving IV iron and at intervals of one to three months routinely
- Iron profile/ferritin in a normal patient annually
17/09/2024
Critical C3 reagent shortage until October
Due to a critical reagent shortage from our supplier, C3 complement will be batch processed twice weekly in order to conserve reagent. This issue is expected to be resolved in early October, 2024. Please note, C4 results will be held back and released alongside C3 result for appropriate clinical comments to be issued. Please contact Cat Dibden (catherine.dibden@nhs.net), Consultant Clinical Scientist for further information, if required.
23/02/2024
As we previously communicated, due to a quality issue with our current (Atellica) reagent, analysis of Erythropoietin (EPO) was paused from 26/01/24. All samples received from this date have been stored appropriately and will be run using the previous (Immulite) method.
The Blood Sciences department will revert back to the previous method for EPO analysis on 27/02/24. This will be on a temporary basis. Please be aware that this method has a slightly different reference range of 4.3-29.0 mIU/mL (compared to 5.5-28.4 mIU/mL) and is not UKAS accredited.
We have been notified by our reagent provider that the Atellica EPO reagent that was in use at BRILS from 09/11/23 – 26/01/24 had a significant negative bias of around -35%. If you have clinical concern that interpretation of your patients’ previous EPO result(s) may have been affected by this, please send a repeat sample for EPO analysis.
Please contact Cat Dibden (Catherine.dibden@nhs.net) if you have any queries or concerns.
09/01/2024
Changes to our urine drugs of abuse service
We are changing how we measure urine drugs of abuse. The test will no longer be performed in-house as we are sending samples to a third-party laboratory. This might have a small impact on the overall turnaround time, but the service will be vastly improved as the repertoire will be massively expanded to include many more substances not previously detected (eg ketamine and atypical antipsychotics), and will also detail specific drugs, rather than just the class of compounds, as has previously been the case for benzodiazepines or amphetamines.
This change will be happening with immediate effect.
If you have any queries about this or any other aspect of our laboratory service, please do not hesitate to contact the lab. iain.woodrow@nhs.net
10/07/2023 Reinstatement of IgA analysis in-house
The issue with supply of reagents for the immunoglobulin A (IgA) assay has been resolved and the test is now restored to the routine test profile for immunoglobulins. One slight change to the service is that immunoglobulin analysis will now be consolidated on the Rotherham site, but this is not expected to affect turn-around time.
12/06/2023 Interpretation of vitamin B12 lower results
The Blood Sciences department is moving onto a new Vitamin B12 reagent lot on 09/06/2023 as the current lot is no longer available. The new lot has shown a noticeable downward shift in results for vitamin B12 concentrations at the lower end of normal, and in some cases these results will now fall below the lower limit of the reference range.
If B12 results are below the reference range without neurological or haematological issues (normal Hb and MCV) consider dietary advice and re-check levels in 6 weeks rather than initiating B12 replacement or undertaking further investigations.
Please contact the Duty Biochemist via switchboard if you have any queries about this change.
27/02/2023 Critical Ferritin reagent shortage until further notice: please only request if clinically indicated
Due to an acute international reagent shortage, we ask that clinicians please only measure ferritin where this will alter management, and the test has not been done in the recent past.
Ferritin requests will be sent to Sheffield Teaching Hospitals Laboratory for analysis from 27/02/2023 onwards while we evaluate an alternative in-house method.
Please note that turn-around times for ferritin results are likely to exceed 24 hours once samples are being sent to Sheffield for analysis. We apologise for any inconvenience this may cause.
For further information, please contact the laboratory or Dr Iain Woodrow on 01226 432772 (ext 2772) or via email (iain.woodrow@nhs.net)
07/02/2023 Consider lead poisoning in children with iron deficiency
A recent case discussion in the BMJ highlighted to need to screen for possible lead poisoning in children who present with pica and/or unexplained iron deficiency. The case reported a child who presented with vomiting under the assumption they had viral tonsillitis, but they deteriorated with no obvious apparent cause. It was five days post-admission that lead was measured and found to be grossly elevated. Despite commencement of chelation therapy, the child did not make a neurological recovery and sadly died. This prompted the laboratory, in collaboration with local paediatricians, to implement a “lead trigger” on the ordering system. Subsequent to introducing this measure, 12 further cases of lead poisoning have been diagnosed.
Following on from this report, we are adding a prompt on ICE to suggest measuring lead in children when ferritin is requested or if pica is part of the presentation.
23/01/2023 Critical Reagent shortage for IgA until mid- to late-February
Due to an acute national reagent shortage, IgA is temporarily removed from the non-invasive liver screen (NILS) and Immunoglobulins profiles to conserve reagent.
IgA will not be available to request directly from ICE, Meditech or via paper requests, but will be added in the laboratory to samples with abnormal tTG or serum protein electrophoresis results suggestive of IgA deficiency. Patients with an IgA monoclone or myeloma DO NOT require IgA measurement as paraprotein concentration is calculated from the Total Protein result. Please only request IgA in the clinical details if urgently indicated by condition and guidelines. If there is a strong clinical need for IgA analysis on your patient, please contact the biochemistry laboratory directly.
This is a temporary measure and we hope to resume our normal procedure as soon as reagent stocks are back to normal. Please note that as of 09/01/2022, expected turn-around times for IgA results will be slightly longer than quoted. The test will only be performed at Rotherham twice-weekly to further conserve reagent. We apologise for any inconvenience this may cause.
For patients with MGUS, please refer to testing frequency in this document: https://www.myeloma.org.uk/wp-content/uploads/2021/09/Myeloma-UK-Myeloma-and-MGUS-A-Guide-for-GPs.pdf
Please do not delay requesting immunoglobulins in those with a clinical suspicion of myeloma, provided the test has not been requested and found to be normal in the preceding 12 months.
For other (non-malignancy) purposes, immunoglobulin testing at a minimum interval of six months is recommended (RCPath National minimum retesting intervals in pathology, 2021).
Please contact the Consultant Biochemist if you require further information.
